Author: Near Me Dental Team
We are a team of talented individuals that take creativity to a new level. We are not just another creative agency, we dream with you. We’re really passionate about our work and we love to turn visions into reality. Our goal is not only to satisfy our clients’ goals, but to exceed them in every way.
Dry Mouth at Night: Common Causes and How to Find Relief – The Ultimate Guide
It’s a familiar and deeply unpleasant sensation: you wake up in the middle of the night, your mouth feeling like a desert. Your tongue is thick and sticky, your lips feel cracked, and you have an urgent, desperate need for a glass of water. For many, this isn’t just an occasional annoyance; it’s a nightly struggle that disrupts sleep and leaves you feeling parched and uncomfortable from the moment you wake up.
While it’s easy to dismiss “dry mouth at night” as a simple thirst problem, it’s often a signal of a deeper issue. This condition, known clinically as xerostomia, is more than just a nuisance. It’s the absence of your mouth’s most critical protective element, and when left unmanaged, it can open the door to a cascade of serious dental problems.
This comprehensive guide is designed to be your definitive resource for understanding and conquering nocturnal dry mouth. We will explore the vital role of saliva, conduct a deep dive into every potential cause—from simple lifestyle habits to complex medical conditions—and provide a complete arsenal of effective dry mouth remedies. Our goal is to empower you with the knowledge to not only find relief but to protect your long-term oral health.
More Than Just Water: The Critical Role of Saliva in Your Mouth
Before we can understand the problem of dryness, we must first appreciate the remarkable substance we so often take for granted: saliva. It’s easy to think of it as just water, but in reality, saliva is a complex, multi-functional fluid—your mouth’s own built-in maintenance system, working 24/7 to keep things in perfect balance.
The Many Jobs of Your Saliva: Your Body’s Unsung Hero
This biological “superfluid” performs a host of essential functions that are critical for your health and comfort:
- It Begins Digestion: Even before food reaches your stomach, saliva starts the digestive process. It contains enzymes like amylase, which begin breaking down starches into simpler sugars right in your mouth.
- It Provides Lubrication: Saliva coats every surface of your mouth, allowing you to speak, chew, and swallow comfortably and effortlessly. Without it, these simple actions would become difficult and painful.
- It Allows You to Taste: You can’t taste what you can’t dissolve. Saliva moistens food, dissolving small particles so they can be detected by the taste buds on your tongue. A dry mouth leads to a dulled sense of taste.
- It Acts as a Constant Cleanser: Throughout the day, saliva gently rinses your teeth, washing away food debris and loose bacteria before they can settle and cause problems.
- It’s a Powerful Acid Buffer: This is one of its most important jobs. After you eat sugary or acidic foods, the bacteria in plaque produce harmful acids. Saliva contains bicarbonate and other compounds that neutralize these acids, bringing your mouth’s pH back to a safe level and protecting your enamel from erosion.
- It Fights Germs: Saliva is packed with powerful antibacterial, antiviral, and antifungal agents, including lysozyme, lactoferrin, and antibodies (like IgA). These components actively seek out and destroy harmful pathogens, preventing infections.
- It Remineralizes Your Teeth: Saliva is supersaturated with calcium and phosphate ions. It constantly delivers these minerals back to the surface of your teeth, helping to repair microscopic lesions and reverse the earliest stages of tooth decay.
What Happens When the Flow Stops? The Dangers of Chronic Xerostomia
When your salivary glands don’t produce enough saliva, this entire protective system breaks down. A chronically dry mouth becomes a welcoming environment for dental diseases to run rampant. The consequences are significant and can progress rapidly:
- Rampant Tooth Decay: Without saliva to wash away food, neutralize acids, and remineralize enamel, your teeth are left defenseless. This can lead to a particularly aggressive form of decay, often starting at the gumline where teeth are most vulnerable.
- Gum Disease (Gingivitis and Periodontitis): Plaque bacteria thrive in a dry environment. The lack of saliva allows plaque to build up quickly along the gumline, leading to inflammation, bleeding (gingivitis), and eventually, the more severe, bone-destroying form of gum disease (periodontitis).
- Oral Infections: Without saliva’s antimicrobial properties, you become much more susceptible to fungal infections like oral thrush (candidiasis), which presents as white, cottage cheese-like patches in the mouth.
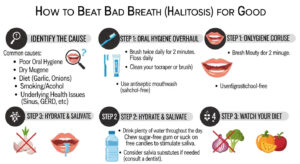
- Persistent Bad Breath (Halitosis): The cleansing action of saliva is key to keeping odor-causing bacteria in check. In a dry mouth, these bacteria multiply, leading to chronic bad breath that mints and mouthwash can’t resolve.
- Pain and Discomfort: A dry mouth can make speaking, chewing, and swallowing difficult. It can also lead to a burning sensation, a cracked tongue, and split lips. For those who wear dentures, the lack of a thin film of saliva can cause painful sores and prevent the dentures from staying in place.
Understanding these stakes is crucial. Dry mouth at night is not a minor inconvenience; it’s a serious health signal that requires your attention.
Decoding the Dryness: A Deep Dive into the Causes of Nocturnal Xerostomia
Finding an effective solution begins with identifying the root cause. The causes of dry mouth are vast and varied, ranging from simple environmental factors to complex medical conditions. Pinpointing why you experience it, especially at night, is the first step toward relief.
Category 1: Lifestyle and Environmental Factors
These factors are often the easiest to identify and modify. They relate directly to your habits and the environment you sleep in.
Mouth Breathing: The Primary Cause of Nighttime Dryness
This is the number one reason people wake up with a severely dry mouth. When you breathe through your mouth instead of your nose, air is constantly passing over your oral tissues, evaporating moisture much faster than your salivary glands can replenish it. You may be a mouth breather at night due to:
- Nasal Congestion: Caused by allergies, a cold, a sinus infection, or other illnesses.
- Anatomical Issues: A deviated septum or nasal polyps can physically block your nasal passages.
- Habit: Some people simply develop the habit of breathing through their mouth, especially during sleep.
Dehydration
Your body cannot produce saliva if it doesn’t have enough water. Even mild dehydration, from not drinking enough fluids throughout the day or from excessive sweating, can significantly reduce saliva production overnight.
Diet and Substance Use
- Alcohol: Alcohol is a diuretic, meaning it causes your body to lose more fluid through urination. It also has a direct dehydrating effect on the tissues in your mouth. A “nightcap” is a common culprit for nocturnal dry mouth.
- Tobacco and Cannabis: All forms of tobacco use can reduce saliva flow and dry out the mouth. Cannabis is also well-known for causing significant xerostomia, often referred to as “cottonmouth.”
- Caffeine: Consuming caffeinated beverages like coffee, tea, or soda, especially in the evening, can have a mild diuretic effect and contribute to dryness.
- Salty or Spicy Foods: Eating very salty or spicy foods close to bedtime can draw moisture out of your oral tissues, leading to a feeling of dryness.
Category 2: The Medication Connection – The #1 Cause of Chronic Xerostomia
If your dry mouth is a persistent, round-the-clock problem that gets worse at night, there is a very high probability that medication is involved. It is estimated that over 500 common medications list dry mouth as a known side effect, and this number climbs to over 1,800 when considering all possible formulations.
These medications don’t directly damage the salivary glands; instead, they often interfere with the nerve signals from the brain that tell the glands to produce saliva. Some of the most common classes of drugs known to cause xerostomia include:
- Mental Health Medications: Antidepressants (especially tricyclics and SSRIs like Zoloft or Prozac), anti-anxiety medications (benzodiazepines), and antipsychotics are major contributors.
- Antihistamines and Decongestants: The very action that dries up a runny nose and sinuses also dries up your mouth. Common culprits include Benadryl, Zyrtec, and Sudafed.
- Blood Pressure and Heart Medications: Diuretics (“water pills”) are designed to remove excess fluid from the body, which reduces saliva. Beta-blockers and other antihypertensives can also be responsible.
- Pain Medications: Both over-the-counter pain relievers (some NSAIDs) and prescription opioids can cause dry mouth.
- Muscle Relaxants and Sedatives: These drugs can affect the central nervous system, impacting saliva flow.
- Medications for Overactive Bladder and Incontinence: These are specifically designed to reduce fluid-related actions in the body.
Category 3: Medical Conditions and Their Treatments
Sometimes, dry mouth is a direct symptom of an underlying medical condition or a side effect of its treatment.
- Autoimmune Diseases: These conditions occur when the body’s immune system mistakenly attacks its own tissues.
- Sjögren’s Syndrome: This is the classic example. The immune system directly attacks the moisture-producing glands, primarily the salivary and tear glands, leading to severe, chronic dry mouth and dry eyes.
- Other Conditions: Rheumatoid arthritis and lupus can also be associated with xerostomia.
- Diabetes: Uncontrolled or poorly controlled diabetes can lead to high blood sugar levels, which can cause dehydration and dry mouth.
- Sleep Apnea: This sleep disorder involves repeated pauses in breathing, often leading to gasping and heavy mouth breathing. Furthermore, the most common treatment, a CPAP machine, can itself be a significant cause of dry mouth as it forces air into the airways.
- Nerve Damage (Neuropathy): Any injury, surgery, or condition that damages the nerves in the head and neck area can disrupt the signals to the salivary glands.
- Cancer Treatments:
- Radiation Therapy: Radiation aimed at the head and neck to treat cancer can severely and often permanently damage the salivary glands, leading to profound xerostomia.
- Chemotherapy: Chemotherapy drugs can affect the whole body, altering the composition and reducing the flow of saliva. This effect is often temporary and resolves after treatment ends.
- Hormonal Changes: Fluctuations in hormones, particularly during menopause, can sometimes lead to a feeling of dryness in the mouth.
- Psychological Factors: Anxiety, stress, and depression can trigger the body’s “fight or flight” response, which naturally reduces saliva flow as the body diverts resources to more critical functions.
Category 4: The Natural Process of Aging
It’s a common misconception that aging itself causes dry mouth. While there can be some age-related changes in salivary gland function, this is not the primary cause. The strong correlation between age and dry mouth is largely because older adults are more likely to have one or more of the chronic medical conditions listed above and are far more likely to be taking multiple medications that cause xerostomia.
Reclaiming Comfort: Your Complete Arsenal of Dry Mouth Remedies
Finding relief from nocturnal dry mouth requires a multi-pronged approach that addresses your specific cause while also managing the symptoms and protecting your oral health. This action plan is your toolkit for fighting back against dryness.
Tier 1: Foundational Lifestyle Adjustments
These are simple, powerful changes you can make to your daily routine and sleeping environment. They are the first line of defense.
- Hydrate Intelligently: Sip water consistently throughout the day—don’t wait until you feel thirsty. Keep a glass or water bottle on your nightstand for immediate relief when you wake up at night.
- Humidify Your Air: This is arguably the most effective remedy for nighttime mouth breathers. Run a cool-mist humidifier in your bedroom at night. This adds moisture to the air you’re breathing, significantly reducing the evaporative effect on your oral tissues.
- Prioritize Nasal Breathing: If you’re a mouth breather, take steps to open your nasal passages. This can include using over-the-counter saline nasal sprays, nasal dilator strips (like Breathe Right), or managing allergies with appropriate medication.
- Stimulate Saliva Flow Naturally: During the day, chew sugar-free gum or suck on sugar-free hard candies. Look for products containing xylitol, a natural sugar substitute that not only stimulates saliva but also inhibits the growth of cavity-causing bacteria.
- Modify Your Diet and Habits: Avoid alcohol, caffeine, and tobacco, especially in the hours before bed. Be mindful of overly salty or spicy foods in your evening meal.
Tier 2: Over-the-Counter (OTC) Solutions for Symptomatic Relief
The pharmacy aisle offers a wide range of products specifically designed to manage the symptoms of xerostomia. These are essential tools for daily comfort.
- Saliva Substitutes (Artificial Saliva): These products do not stimulate your own saliva but instead provide lubrication to mimic its effects. They come in various forms:
- Sprays: Convenient for quick, on-the-go relief.
- Rinses: Good for coating the entire mouth before bed.
- Gels: Thicker and more long-lasting, ideal for applying directly to gums and the tongue right at bedtime for overnight protection.
- Moisturizing Mouthwashes and Rinses: Look for products specifically labeled for dry mouth (e.g., from brands like Biotène, ACT, or TheraBreath). These are formulated with enzymes, lubricants, and moisturizers. **Crucially, they must be alcohol-free**, as alcohol will only worsen the dryness.
- Adhering Discs for Overnight Use (e.g., XyliMelts): These are a game-changer for nocturnal dry mouth. They are small, adhesive discs that you stick to your gums or teeth. They slowly dissolve over several hours while you sleep, continuously releasing xylitol and a lubricant to keep your mouth moist.
- Xylitol-Based Products: Beyond gum and melts, look for xylitol in toothpastes, mints, and sprays. It provides moisturizing benefits while actively fighting decay.
Tier 3: The Non-Negotiable Oral Hygiene Protocol for Protection
This is not just a remedy; it is an absolute necessity to prevent the devastating dental consequences of xerostomia.
- Aggressive Fluoride Use: Fluoride is your best friend. Use a prescription-strength fluoride toothpaste (like Prevident 5000) recommended by your dentist. Follow up with a daily, alcohol-free fluoride rinse to constantly strengthen your enamel.
- Impeccable Cleaning: You must be extra diligent with your brushing and flossing. Consider an electric toothbrush to ensure thorough plaque removal. Floss every single day without fail, as the area between teeth is highly vulnerable.
- More Frequent Dental Visits: A person with chronic dry mouth cannot follow the standard six-month recall schedule. Your dentist and hygienist will likely recommend check-ups and professional cleanings every three to four months to stay ahead of tartar buildup and catch any early signs of decay.
Tier 4: Professional and Prescription Interventions
When lifestyle changes and OTC products aren’t enough, it’s time to work with your medical and dental professionals on more advanced solutions.
- Medication Review and Adjustment: This is a critical conversation to have with the medical doctor who prescribed your medications. Never stop or change the dose of a prescribed medication on your own. Your doctor may be able to:
- Adjust the dosage.
- Change the timing of the dose.
- Switch you to an alternative medication in the same class that has a lower likelihood of causing dry mouth.
- Prescription Saliva Stimulants (Sialagogues): For patients with functioning salivary gland tissue (often those with Sjögren’s Syndrome or radiation-induced xerostomia), doctors can prescribe medications that stimulate the glands to produce more saliva. The two most common are:
- Pilocarpine (brand name Salagen)
- Cevimeline (brand name Evoxac)
These can be very effective but also have systemic side effects (like sweating and flushing) that require management by a physician.
Don’t Go It Alone: Why Your Dentist Is Your Best Ally Against Xerostomia
It’s tempting to try and manage dry mouth all on your own, but this approach can be risky. Your dentist and dental hygienist are not just there to fix the problems caused by dry mouth; they are your primary partners in diagnosing, managing, and preventing its complications.
A skilled dentist or hygienist at a trusted dental clinic is often the very first healthcare professional to notice the subtle, early signs of xerostomia—like a lack of saliva pooling on the floor of the mouth, or a “lipstick sign” where lipstick sticks to the front teeth. They are your “dry mouth detectives.”
During your exam, they will:
- Help you pinpoint potential causes by thoroughly reviewing your health history and medications.
- Assess the extent of the impact on your oral health.
- Provide personalized recommendations for the most effective OTC products for you.
- Prescribe the necessary high-strength fluoride toothpaste or rinses to protect your teeth.
- Establish the appropriate, more frequent schedule for cleanings and check-ups.
- Communicate with your primary care physician to create a collaborative healthcare plan, especially if medication adjustments are needed.
If the damage from dry mouth has already occurred, such as cavities or worn enamel, your dental team, including a cosmetic dentist, can provide restorative treatments to repair your smile and protect it from further harm.
The Expert Consensus on Managing Xerostomia
The entire healthcare community recognizes the seriousness of dry mouth. The American Dental Association (ADA) provides extensive resources for both patients and professionals, stressing that managing xerostomia is critical for preventing “oral diseases such as caries and periodontitis.” For those whose dry mouth is caused by a specific condition like Sjögren’s Syndrome, organizations like the Sjögren’s Foundation offer invaluable support and information, underscoring the need for a multidisciplinary approach involving both medical and dental care.
Conclusion: Your Path to a Comfortable and Healthy Mouth
Waking up with dry mouth at night is a problem that should never be ignored. It’s a sign that your mouth’s natural defenses are down, leaving your teeth and gums vulnerable. While the list of potential causes of dry mouth is long, the list of effective dry mouth remedies is equally robust and empowering.
The journey to relief is a partnership between you and your healthcare team. Your role is to implement the foundational lifestyle changes—hydrating, humidifying your environment, and using effective OTC products. Your dentist’s role is to be your expert guide, providing professional protection, personalized recommendations, and the crucial oversight needed to keep your mouth healthy.
You do not have to live with the constant discomfort of dryness or the anxiety of potential dental damage. You can take control, find comfort, and secure the long-term health of your smile.
Ready to find lasting relief and protect your smile from the dangers of xerostomia? Don’t wait for a small problem to become a big one. Use the Near Me Dental directory to find a compassionate, knowledgeable dental team in your area and book a consultation today.