Author: Near Me Dental Team
We are a team of talented individuals that take creativity to a new level. We are not just another creative agency, we dream with you. We’re really passionate about our work and we love to turn visions into reality. Our goal is not only to satisfy our clients’ goals, but to exceed them in every way.
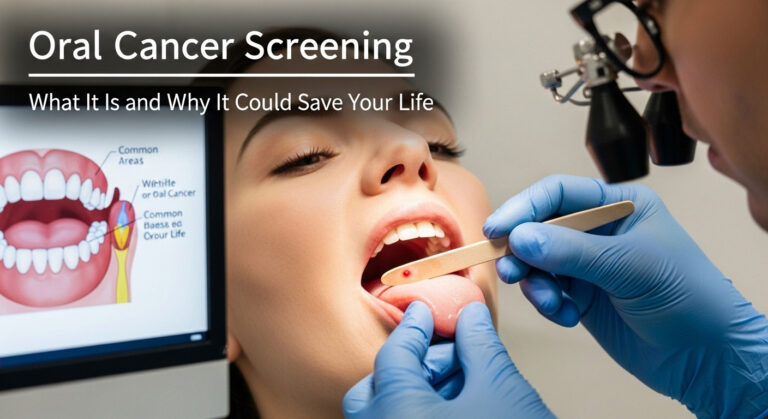
Oral Cancer Screening: What It Is and Why This Simple Exam Could Save Your Life
When you schedule a dental appointment, your mind likely goes to the familiar: the whir of the polisher, the quick check for cavities, the gentle reminder to floss more. You think about getting a clean, bright smile. But behind the scenes of that routine visit, your dentist is performing one of the most important health checks you can receive—one that has nothing to do with fillings and everything to do with saving your life.
This is the oral cancer screening. It’s a quick, painless part of a regular dental check-up that many patients don’t even realize is happening. Yet, its importance cannot be overstated. The key to surviving oral cancer isn’t found in complex treatments, but in a single, powerful action: early detection. When found in its earliest stages, oral cancer has a remarkably high survival rate. When found late, that rate plummets dramatically.
This guide is designed to pull back the curtain on this vital procedure. We will demystify the entire process, help you understand the critical oral cancer signs, identify the key risk factors, and explain why a routine dentist cancer screening is the cornerstone of proactive preventive care. This isn’t meant to cause fear, but to empower you with knowledge—the most powerful tool you have to protect your health.
What Is Oral Cancer? A Clear and Simple Explanation
In the simplest terms, oral cancer is an uncontrolled growth of abnormal cells in the mouth or throat. Like other cancers, it occurs when the normal life cycle of cells is disrupted, causing them to multiply without limit and form tumors. These cancers fall under a broader category called “head and neck cancers.”
Where Can Oral Cancer Develop?
The term “oral cancer” can refer to cancer in any of several locations. Understanding these areas helps make the abstract concept more tangible:
- The Lips: Most often on the lower lip, commonly linked to sun exposure.
- The Tongue: Particularly on the sides and the underside of the tongue.
- The Floor of the Mouth: The area underneath the tongue.
- The Buccal Mucosa: The inner lining of the cheeks.
- The Gums (Gingiva): The tissue surrounding the teeth.
- The Palate: Both the bony “hard palate” at the front of the roof of the mouth and the fleshy “soft palate” at the back.
- The Oropharynx: The part of the throat just behind the mouth, which includes the back third of the tongue, the soft palate, the side and back walls of the throat, and the tonsils. Cancers in this area, particularly those linked to HPV, are on the rise.
The Critical Importance of Early Detection: A Tale of Two Outcomes
The entire purpose of a screening is to find cancer or pre-cancerous conditions early, before they cause symptoms and when treatment is most effective. The difference between early and late detection for oral cancer is stark and life-altering.
Think of it like discovering a weed in your garden. If you find a tiny sprout (an early-stage lesion), you can easily pluck it out with minimal effort and no damage to the surrounding garden. If you let that weed grow for months until it becomes a large, deeply rooted bush (a late-stage tumor), removing it becomes a far more difficult and destructive process, leaving a significant impact on the garden’s health and appearance.
The statistics bear this out. According to the Oral Cancer Foundation, the five-year survival rate for those with an early-stage, localized diagnosis is approximately 85%. If the cancer is not found until it has spread to other parts of the body (metastasized), that survival rate drops to around 39%. A screening aims to catch it in that 85% window.
The Unseen Hero: Understanding the Dentist Cancer Screening Process
The most important thing to know about a dentist cancer screening is that it is a quick, comfortable, and non-invasive part of a comprehensive dental exam. There are no special preparations needed. Your dentist or hygienist performs this vital check as a natural extension of looking at your teeth and gums.
The Conventional Visual and Tactile Exam: The Gold Standard
This hands-on examination is the most reliable and effective method for screening. It involves both looking (visual inspection) and feeling (palpation). Here is a step-by-step walkthrough to demystify what’s happening.
Step 1: The Health History Conversation
Your screening begins with a conversation. Your dentist will ask about your health history, lifestyle, and any new symptoms you may have noticed. Be prepared to answer questions honestly about:
- Tobacco and alcohol use (frequency and duration).
- Any new lumps, bumps, or sores you’ve noticed.
- Any difficulty or pain with chewing or swallowing.
- Your sun exposure habits.
- Your HPV vaccination status.
This information helps the dentist assess your personal risk profile.
Step 2: The Face, Head, and Neck Exam (Extra-oral)
Before even looking in your mouth, your dentist will examine your head and neck from the outside. They are looking for visual signs of asymmetry, swelling, or skin changes. They will then gently use their fingertips to feel your neck (along your lymph node chains), under your jaw, and around your salivary glands, checking for any unusual firmness, lumps, or tenderness. This is a crucial step, as swollen lymph nodes can sometimes be the first detectable sign of a problem.
Step 3: The Lip and Cheek Exam (Intra-oral)
Now the exam moves inside your mouth. Your dentist will ask you to relax your mouth as they gently pull your upper and lower lips out and away from your gums, inspecting the inner surfaces for any sores or changes in color or texture. They will do the same for your inner cheeks (your buccal mucosa).
Step 4: The Gum and Palate Exam
They will meticulously examine all of your gum tissue, looking for any abnormal spots. They will then have you tilt your head back to get a clear view of the entire roof of your mouth, checking both the hard and soft palate.
Step 5: The Tongue Exam
This is one of the most critical parts of the screening, as the tongue is a very common site for oral cancer. To do this properly, the dentist will take a small, dry piece of gauze to gently hold the tip of your tongue. This allows them to:
- Have you stick your tongue straight out to examine the top surface.
- Gently pull the tongue to your left to get a clear view of its entire right side.
- Gently pull the tongue to your right to see the entire left side.
- Have you touch the tip of your tongue to the roof of your mouth to examine the entire underside.
This process is gentle and allows for a thorough inspection of all surfaces, which is impossible to do on your own.
Step 6: The Floor of the Mouth Exam
While your tongue is still lifted, the dentist will inspect the floor of your mouth—the U-shaped area underneath the tongue. They will also gently press one finger inside and one finger outside under your chin to feel for any lumps in this area.
Is It Painful? Is It Scary?
Absolutely not. This entire process is painless. It is simply a very thorough process of looking and feeling. A skilled and compassionate dentist will explain what they are doing as they go, making the experience feel routine and comfortable. The entire hands-on screening often takes only two to three minutes but provides an immense amount of valuable information.
Advanced Screening Technologies: A Deeper Look
In addition to the standard visual and tactile exam, you may see some dental offices using advanced adjunctive tools designed to enhance their screening capabilities. It’s important to understand what these are and what their role is.
Fluorescent Light Technology (e.g., VELscope, Identafi)
These devices are becoming increasingly common. They work on the principle of tissue fluorescence.
- How It Works: The device emits a specific wavelength of harmless blue light into the mouth. Under this light, healthy oral tissue naturally fluoresces and appears as a bright green color through a special filter. However, areas of abnormal tissue, which have undergone metabolic or structural changes (such as pre-cancer or cancer), do not fluoresce in the same way and appear as dark, irregular patches.
- What It’s For: It’s crucial to understand that this is an *adjunctive screening tool*, not a diagnostic one. It helps the dentist to visualize potential abnormalities that might be subtle or invisible to the naked eye and can help define the margins of a visible lesion. A dark spot does NOT mean you have cancer; it simply means that area warrants closer inspection.
Toluidine Blue Stain
This is an older but still occasionally used technique. It involves having the patient rinse with a special blue dye.
- How It Works: After rinsing, abnormal cells (which have larger nuclei) tend to absorb more of the dye and will stain a dark royal blue, while healthy tissues will be lightly stained or not at all.
- What It’s For: Like fluorescence, this is an aid, not a diagnosis. It can help a dentist decide if a biopsy is warranted and can help identify the best location from which to take a tissue sample.
Are These Advanced Tools Necessary? A Balanced Perspective
The gold standard for oral cancer screening remains the thorough, conventional visual and tactile exam performed by an experienced clinician. The ADA and other professional bodies do not currently mandate the use of these adjunctive devices, as there is ongoing research to determine their precise impact on patient outcomes.
While they can be helpful in some situations, they can also produce “false positives,” where a benign inflammation or irritation might appear dark, causing unnecessary anxiety. The most important factor is the skill and diligence of your dentist. Think of these tools as a helpful flashlight, but your dentist’s brain and experience are the true engine of the screening.
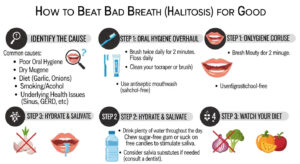
Recognizing the Red Flags: A Comprehensive Guide to Oral Cancer Signs
One of the most powerful things you can do for your health is to be an active, educated participant. While your dentist performs the professional screening, you are the one who lives with your body every day. Knowing the oral cancer signs allows you to spot potential issues between visits. The key is the two-week rule: any new or unusual sign or symptom that does not resolve on its own within two weeks should be professionally evaluated.
The Most Common Signs and Symptoms to Be Aware Of:
- A Sore That Won’t Heal: This is the most common sign. A sore, ulcer, or irritation in your mouth or on your lip that bleeds easily and does not show significant healing after 14 days is a major red flag.
- A Red or White Patch (Erythroplakia or Leukoplakia):
- Leukoplakia: A white or grayish patch that cannot be wiped away.
- Erythroplakia: A flat or slightly raised, velvety red patch. Red patches are generally less common but have a much higher potential to be pre-cancerous.
- Erythroleukoplakia: A patch with both red and white areas.
- A Lump, Bump, or Thickening: Any new lump or thickening of the skin or lining inside your mouth, or a lump in your neck.
- Pain, Tenderness, or Numbness: Any unexplained and persistent pain or numbness in the mouth, lips, or face.
- Difficulty with Function: New or persistent difficulty chewing, swallowing, speaking, or moving your jaw or tongue.
- A Feeling of Something Caught in the Throat: A constant sensation that something is stuck in your throat is a key potential sign of oropharyngeal cancer.
- Voice Changes: Unexplained hoarseness or a change in your voice that lasts for more than two weeks.
- A Change in Your Bite: A sudden feeling that your teeth or dentures no longer fit together correctly.
- Unexplained Bleeding: Any spontaneous bleeding in the mouth not related to an obvious injury.
- Ear Pain: A persistent pain in one ear without any associated hearing loss can sometimes be “referred pain” from a tumor in the throat.
The Importance of Self-Exams: Your Role in Early Detection
You can and should perform a monthly self-exam at home. It only takes a minute and can help you become familiar with what’s normal for your mouth, making it easier to spot changes. All you need is a bright light and a mirror.
- Face and Neck: Look at your face in the mirror for any swelling or asymmetry. Gently press along the sides and front of your neck, feeling for any lumps.
- Lips and Cheeks: Pull out your lips and check the inner surfaces. Pull out your cheeks and look at the lining.
- Gums: Lift your lips to see all your gum tissue, front and back.
- Roof of Mouth: Tilt your head back and say “Ahh” to see the entire hard and soft palate.
- Tongue: Stick your tongue out and look at the top. Then, using a clean cloth or gauze, gently hold the tip and pull it to each side to see the lateral borders. Finally, touch the tip of your tongue to the roof of your mouth to examine the entire underside.
A self-exam is not a substitute for a professional screening, but it is a powerful partnership.
Understanding Your Risk: Key Factors for Oral Cancer
While oral cancer can affect anyone, certain factors significantly increase a person’s risk. Understanding these can help you and your dentist assess your personal situation.
The “Traditional” High-Risk Factors
- Tobacco Use: This is the single greatest risk factor. All forms of tobacco—cigarettes, cigars, pipes, and smokeless tobacco (chew, snuff, dip)—contain dozens of known carcinogens that directly damage the cells in the mouth and throat.
- Heavy Alcohol Consumption:
- Age:
- Excessive Sun Exposure:
The New and Growing Risk Factor: HPV
This is a critical piece of the modern oral cancer puzzle. The Human Papillomavirus (HPV), specifically HPV-16, has emerged as a leading cause of oropharyngeal cancers (those in the tonsils and at the base of the tongue).
- What to Know about HPV-Related Cancers:
- A Different Demographic: Unlike traditional oral cancers, HPV-related cancers often affect a younger, healthier, non-smoking population. The myth that oral cancer is only a disease of old smokers is dangerously outdated.
- Location: They most commonly occur in the hard-to-see oropharynx, making a professional screening even more vital.
- Symptoms: The signs are often subtle, such as a persistent sore throat, a painless lump in the neck, or unilateral ear pain.
- Prognosis: The good news is that HPV-positive oropharyngeal cancers generally respond much better to treatment and have a significantly higher survival rate than HPV-negative cancers.
Other Contributing Factors
Other factors that can play a role include a weakened immune system (due to certain diseases or immunosuppressant drugs), poor nutrition (a diet low in fruits and vegetables), and a personal or family history of head and neck cancer.
“My Dentist Found Something.” What Happens Next? An Anxiety-Free Guide
Hearing your dentist say, “I see a spot here I’d like to keep an eye on,” can be terrifying. It’s important to understand that this is the beginning of a careful, methodical process, not an immediate diagnosis of cancer. Panicking is a natural response, but here is what to expect.
- Observation and Re-evaluation (The Two-Week Rule): The vast majority of sores, spots, and irritations in the mouth are benign and caused by simple trauma (like biting your cheek), a canker sore, or a herpes lesion. The first and most common step is for your dentist to document the finding and ask you to return in two weeks. This gives the spot time to heal on its own. If it’s gone at the follow-up, the case is closed.
- The Referral to a Specialist: If the lesion has not healed or has changed in appearance after two weeks, your dentist will refer you to a specialist for a definitive diagnosis. This is most often an oral surgeon or an otolaryngologist (ENT). This referral is a sign of caution and good practice, not a confirmation of cancer.
- The Biopsy – The Only Way to Know for Sure: The specialist will likely recommend a biopsy. This is the only way to get a definitive diagnosis. It’s a minor surgical procedure where a small sample of the suspicious tissue is removed and sent to a pathologist for microscopic analysis. It’s typically done right in the surgeon’s office with local anesthetic and is a quick and comfortable process.
- Getting the Results and Making a Plan: The pathologist’s report will classify the tissue. It may be benign (non-cancerous), dysplasia (pre-cancerous), or carcinoma (cancerous). Even a finding of “dysplasia” is a major win for early detection, as it means the abnormal cells can be removed before they have a chance to turn into invasive cancer. Based on the results, the specialist will discuss the next steps, which could range from continued observation to further treatment.
Finding Your Partner in Preventive Health: The Role of Your Dentist
Your dentist is far more than a “tooth mechanic.” They are primary healthcare providers and your first line of defense in the fight against oral cancer. They are trained to see the subtle changes in your mouth that you would never notice. Establishing a long-term, trusting relationship with a dentist and their team at a quality dental clinic is one of the most important things you can do for your health.
The oral cancer screening is an integral, standard part of every comprehensive dental exam they provide. It embodies the very essence of preventive care: taking proactive steps to stop a disease before it can become a life-threatening problem. They are your health partner, your expert screener, and your gateway to specialized care if it’s ever needed.
The Authoritative Stance: What the Experts Say
The entire healthcare community is united on the importance of this issue. Citing the immense difference in outcomes, the Oral Cancer Foundation states that “early detection… is the key to survival.” The American Cancer Society provides extensive information on risk factors and signs, empowering the public with knowledge. Furthermore, the American Dental Association (ADA) firmly advocates for dentists to perform these screenings as a routine and essential component of patient care, recognizing their unique position to identify this disease in its earliest stages.
Conclusion: The Most Important Two Minutes of Your Dental Visit
Your regular dental visit is an opportunity for so much more than a cleaning. It’s a comprehensive health check, and the oral cancer screening is its most vital, life-saving component. This quick, painless, and simple examination is your single best tool for detecting oral cancer in its infancy when it is most treatable and survivable.
You are a crucial part of this process. By understanding the risk factors, performing monthly self-exams, and knowing the warning signs, you become an active partner with your dentist in guarding your health. Don’t let fear or complacency keep you from this essential preventive care.
View your next dental appointment not as an errand, but as a profound investment in your future. If it has been a while since your last comprehensive exam, or if you’ve never had a dedicated oral cancer screening, the time to act is now. Your health is your most precious asset. Protect it.
Use the Near Me Dental directory to find a compassionate, thorough dentist in your area who makes preventive care a priority, and book your potentially life-saving screening today.